Reversal Nightmare: Unsolved Questions


(Disclaimers - drug Images are taken from google images and not related to the story narrated in the blog )
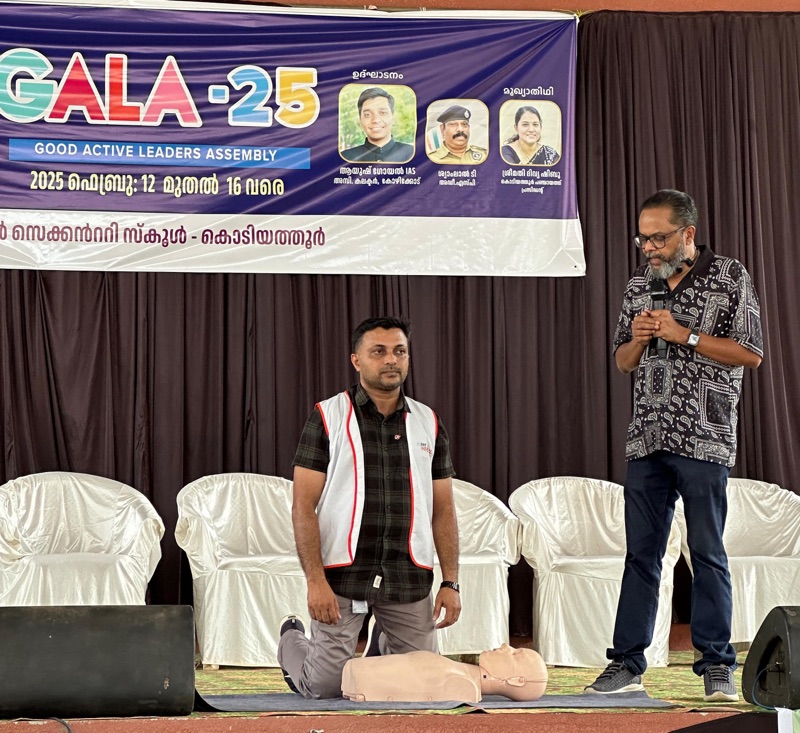
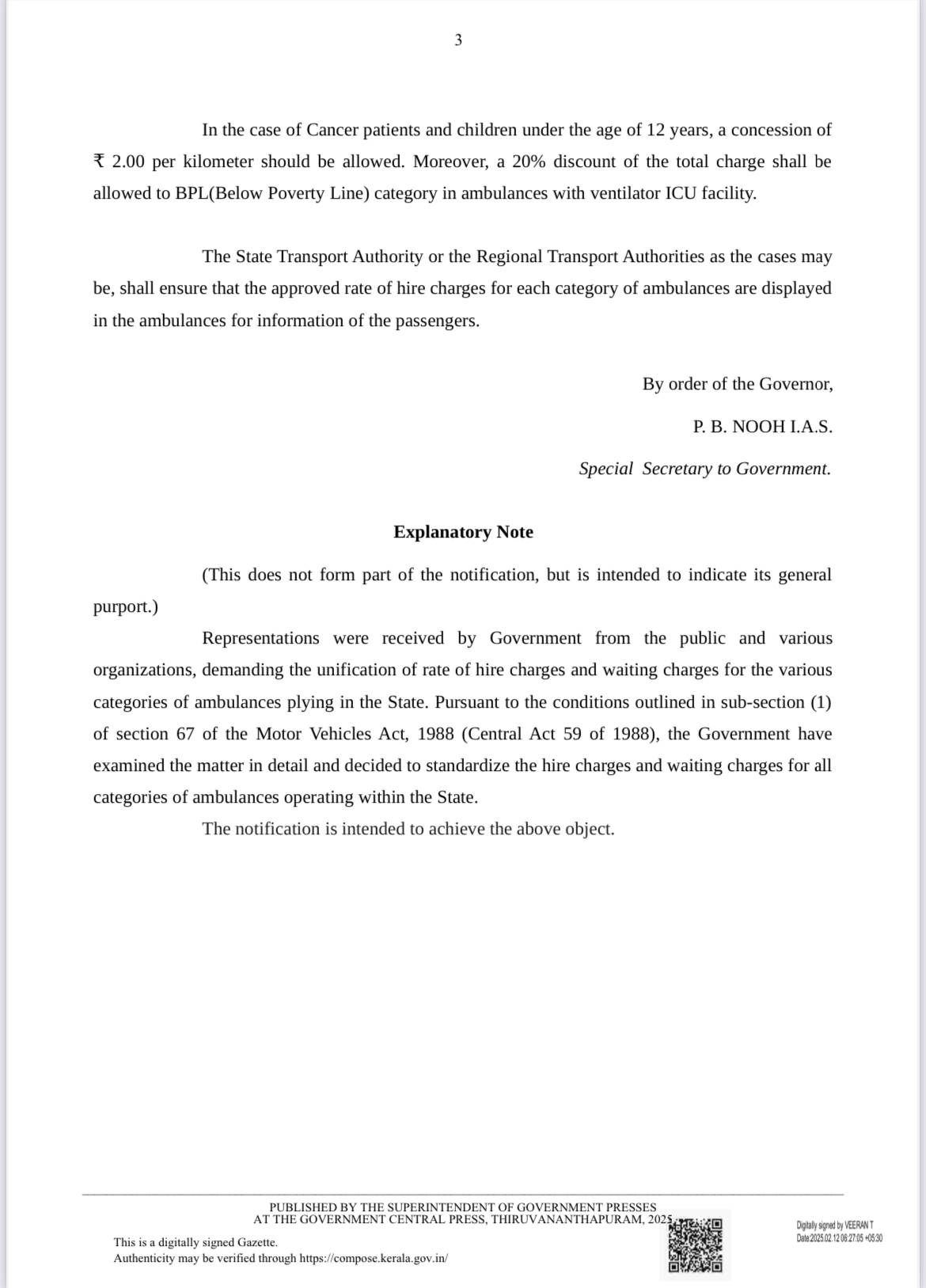
In the year of 1990s and then , as we embarked on our anesthesia careers, we took immense pride in being mentored by the esteemed Prof. M.R. Rajagopal, often hailed as the father of modern anesthesia in Kerala. Our operating theaters (OTs) lacked the advanced monitoring equipment we have today; even a basic cardiac monitor was considered a luxury. We relied on the fundamentals: feeling the pulse with our fingers, placing the stethoscope bell on the patient’s chest, and keeping the earpieces in our ears” -these were our gold standards.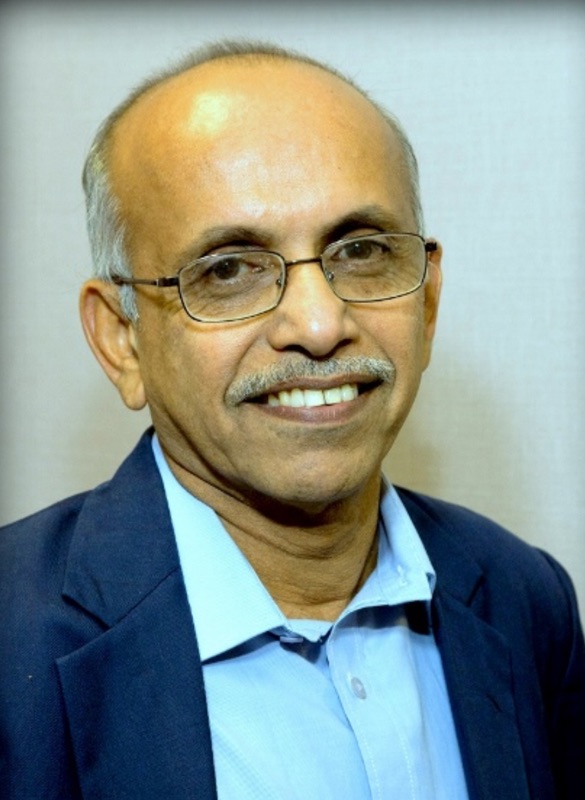
Prof MR Rajagopal
I vividly recall the excitement surrounding the arrival of Kerala’s first pulse oximeter at Calicut Medical College’s Anesthesia Department. Prof. Rajagopal demonstrated its unique, life-saving capabilities. At that time, such a device cost around one lakh rupees. Today, pulse oximeters are ubiquitous, found in homes and even integrated into smartwatches” - a transformation accelerated by the COVID-19 pandemic.
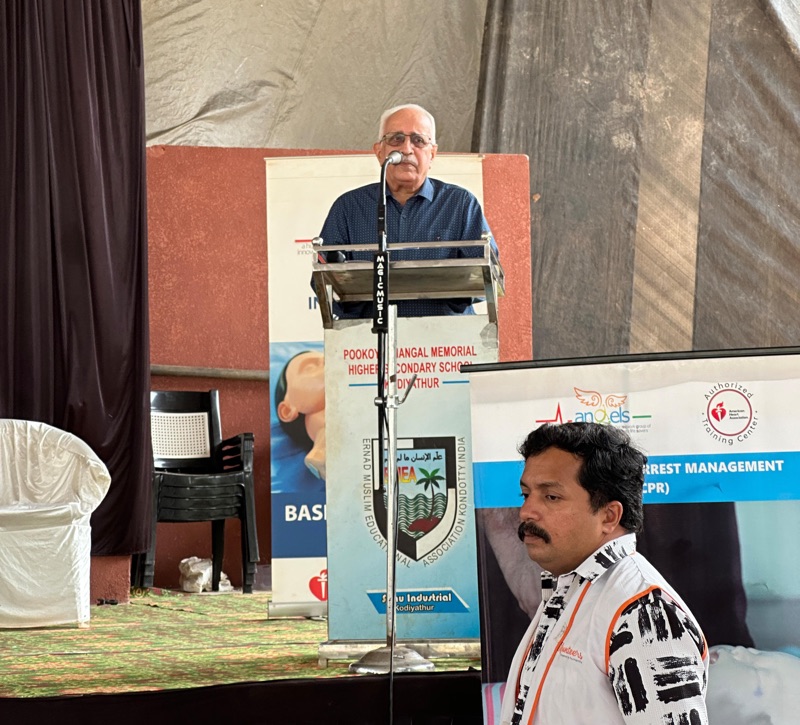
Against this backdrop, I recount a harrowing experience that befell many anesthesiologists, particularly freelancers. Dr. Suresh Kumar K. played a pivotal role in unraveling the mystery behind these distressing events when he was working in a leading private hospital in Kozhikode.
The Incident
Dr. Suresh administered general anesthesia (GA) for a thyroid surgery after a thorough pre-anesthesia check. Fortunately, a cardiac monitor was available during the procedure. The standard practice of the 1990s was followed: induction with thiopentone, intubation under suxamethonium, maintenance with oxygen, nitrous oxide, halothane, and pancuronium as a long-acting muscle relaxant. At the surgery’s conclusion, reversal was achieved using five ampoules of neostigmine combined with two ampoules of atropine to counteract neostigmine’s muscarinic effects.
Dr Suresh Kumar K
Unexpectedly, the patient developed tachycardia, hypertension, ventricular ectopics, and pulmonary edema following the reversal. Dr. Suresh was perplexed; despite meticulous anesthesia management, these complications arose in a young, ASA grade 1 patient without comorbidities. He meticulously reviewed every step but found no errors. Thankfully, he managed the adverse events with appropriate interventions.
Determined to find answers, Dr. Suresh seized all medications used during the procedure, categorized them by batch, and sent samples to a trusted laboratory for analysis.
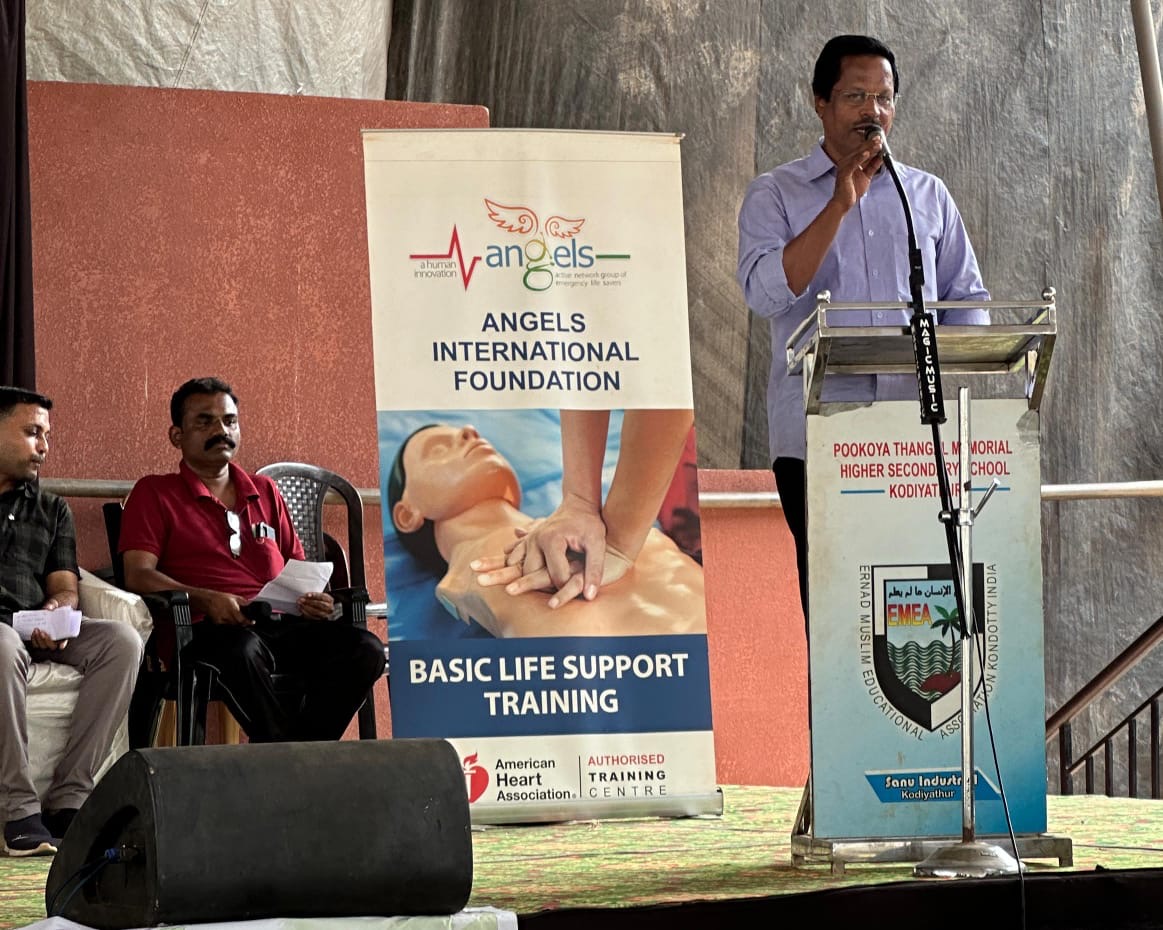
A Disturbing Pattern Emerges
In the interim, Dr. Suresh presented the case at an anesthesiologist’s forum, seeking insights from peers. Alarmingly, over 15 freelance anesthesiologists shared similar experiences- clinical disasters during anesthesia sessions. Tragically, many of these cases lacked proper pre-anesthesia checks and monitoring. Most resulted in patient deaths, with anesthesiologists attributing the outcomes to their own mistakes. These incidents were often recorded as cardiac arrests due to underlying cardiovascular diseases.
The Revelation
During this period, Dr. Suresh received the laboratory analysis reports. Neostigmine, pancuronium, suxamethonium, and thiopentone were all within normal parameters. However, the analysis of the atropine ampoules was shocking: they contained adrenaline.
Adrenaline is a life-saving drug in critical situations like acute cardiac arrest, acute anaphylaxis, and acute severe bronchial asthma- a fact we were taught meticulously by Prof. Hariharan, our veteran pharmacology instructor. However, when administered inadvertently in place of atropine during anesthesia reversal, adrenaline can precipitate severe cardiovascular complications, as observed in Dr. Suresh’s patient.
Unanswered Questions
This discovery raised several unsettling questions:
1- How did adrenaline come to be mislabeled as atropine?
2- Were there lapses in the pharmaceutical manufacturing process?
3- How widespread was this issue?
4-How many patients suffered or even died due to this error?
5-What measures could be implemented to prevent such incidents in the future?
A Call to Action
Dr. Suresh’s relentless pursuit of the truth not only unveiled a critical pharmaceutical error but also underscored the importance of vigilance, thorough investigation, and open communication within the medical community. This incident serves as a stark reminder of the potential consequences of medication errors and the need for stringent quality control in drug manufacturing.
As we reflect on this episode, it is imperative that we, as healthcare professionals, advocate for:
1)Rigorous quality assurance protocols in pharmaceutical production.
2)Comprehensive reporting and analysis of adverse events.
3)Continuous education and training to recognize and manage unexpected intraoperative complications.
Only through such collective efforts can we hope to prevent similar nightmares in the future and ensure the safety and well-being of our patients.